The Real Impact of Budget Cuts to Aged Care

In a Nutshell: The Impact of Budget Cuts to Aged Care #2
Summary:
In our first analysis of the impacts of the 2016 Budget, we described an unbalanced budget that sought to find short term savings from a sector that urgently requires greater investment.
Our clinical and operations team has now had the opportunity to comprehensively evaluate the proposed changes to the funding instrument. This report highlights major concerns requiring urgent attention:
- The Government has sought to claw back over $1.7 billion over the next 4 years, focusing on the complex care domain. This represents a direct cut in funding to the most disadvantaged Australians, particularly those suffering from chronic pain, degenerative disease, severe arthritis and complex wounds.
- Modifications proposed to the ACFI funding instrument are projected to result in cuts of $350 million in excess of those announced by Government in the budget and Mid-Year Economic and Fiscal Outlook (MYEFO).
- While the cuts compromise the viability of the sector, the threats to the vulnerable aged are even more concerning. The ACFI changes create a disincentive to admit high dependency people and will ultimately result in their displacement to hospitals.
We believe that it is critical that the aged care and broader healthcare sector work collaboratively with Government to ensure that these changes do not proceed.
Targeting Funding Cuts to the Most Vulnerable Residents
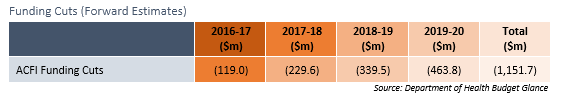
Key to the aged care budget announcement were cuts to Aged Care Funding Instrument (ACFI) funding for the care of residential care clients with Complex Health Care (CHC) needs. The Government expects to claw back close to $1.2 billion over the next four years in addition to the $607 million cuts announced in the Mid-Year Economic and Fiscal Outlook.
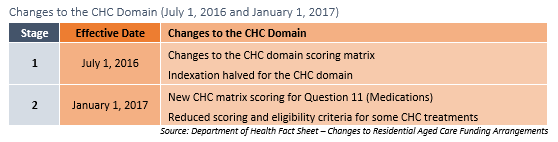
CHC includes medication assistance, pain treatments and other care interventions for the most frail and unwell residents living in residential care. The changes will be implemented in two stages over the coming six months.
The changes will only affect new or reclassified residents. Given that residents included in the CHC domain are generally the most frail and complex and have short lengths of stay, it is anticipated that the changes will affect most residents within a short period of time.
July 1, 2016 Changes
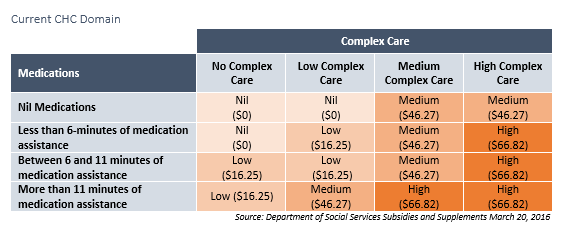
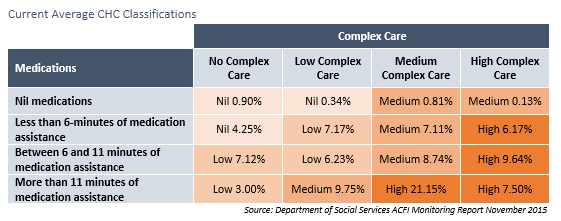
The existing scoring matrix comprises both the medication and complex care domains, medication assistance and complex care treatments.
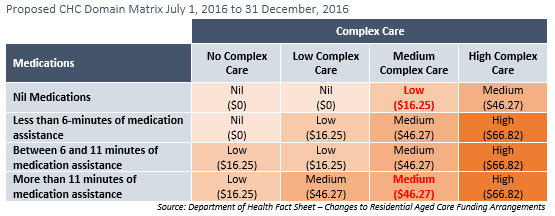
The proposed tool results in the “downgrade” of two categories in the CHC domain:
- Score for a rating of D in Question 11 (Medication) and a C in Question 12 (CHC) will be reduced from 3 points to 2 points; and
- Score for a rating of A in Q11 and a C in Question 12 will be reduced from 2 points to 1 point.
The changes will result in an average loss of $4.62 per day for every new care recipient and will result in funding cuts of $67,600 to the average 80-bed home in the next six-months. The January 1, 2017 changes will be far more profound.
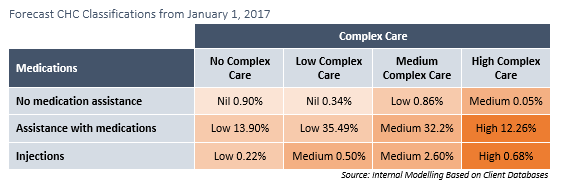
January 1, 2017 Changes to Medication Scoring
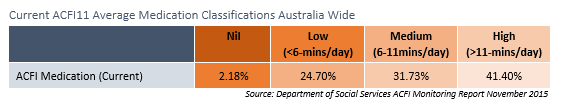
Current ACFI funding for medication assistance is based on the timing of medications. Four categories, ranging from no care needs to high care needs classify the care requirements of each resident. Currently residents who require over 11-minutes each day or who receive regular injections are considered to have “high” care needs. Over 40% of residents fall into this classification Australia wide.
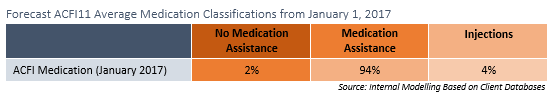
Changes announced by the Department of Health following the 2016-17 budget have described a new system for classifying medication assistance. The new classification will be reduced to three rating based on the requirement for assistance, not the time taken to assist the resident. Residents will either be classified as requiring:
- No assistance needed with medications;
- Assistance needed with medications; or
- Injections (subcutaneous, intramuscular, intravenous).
Our analysis indicated that this change will result in a significant shift in funding well in excess of forward estimates. Initial research on typical facilities throughout Australia indicates that approximately 4% of residents receive regular injections. This is predominantly for the treatment of insulin-dependent diabetes. Australia wide, only one in every one-hundred thousand Australians are insulin dependent diabetics. The higher rate in residential aged care is reflective of the age and medical complexity of residential care recipients.
Given that the rate of residents who do not require medications will not change classifications, close to 95% of residents will fall into the “medication assistance” classification. There will be a ten-fold decrease in the number of residents’ falling into the highest classification.
We predict that the changes to medication administration classification will have a profound impact on the funding of vulnerable residents who have the highest care needs.
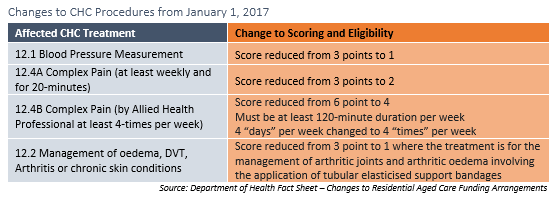
January 1, 2017 Changes to CHC Scoring and Eligibility
From July 1, 2017 changes will also be made to the scores and eligibility requirements for some complex care treatments:
Data from the Department of Social Services shows that 44.59% of residents are currently receiving an overall high CHC score. The majority of these residents receive treatments to alleviate pain.
Our initial research across multiple sites indicates that the effect of these changes will be profound on the funding of residents with high care needs. Estimates indicate that less than 13% of residents will be classified as having high complex health needs following the January 1, 2017 changes. This represents a three times reduction.
Our calculations, based on the information provided in the ACFI Monitoring Report and the Department of Health’s 2014/15 Report on the Operation of the Aged Care Act 1997, indicates that residents are currently funded an average of $45.84 per day for the care of CHC needs. Our analysis indicates that this will reduce to an average of $30.80 per day for residents who enter care following the implementation of the proposed changes in 2017. The changes will be more profound for homes that have an increased focus on 12.4B pain treatments.
An average 80-bed home will lose $439,000 in funding each year following the change.
Projected Funding Cuts
The budget claw back, announced in Budget 2016-17 of $1.1 billion, is exclusive of funding cuts announced in February 2016 through the Mid-Year Economic and Fiscal Outlook (MYEFO) of $607 million, creating an aggregate reduction of $1.71 billion over the next four years.
Based on the announced changes to the CHC Domain, Ansell Strategic have projected funding cuts across four years. Although the length of stay of the most complex residents is shorter than less frail residents, we have conservatively projected changes against the average length of stay of 34.5 months published by the Australian Institute of Health and Welfare.
We estimate that the proposed changes to the ACFI Instrument will deliver funding cuts of almost $350 million more than projected by the Government. Our analysis indicates that funding claw backs to providers will be in excess of $2 billion over the next four years alone. As the proposed changes are permanent, there will be long term ramifications for the most vulnerable residents and the providers that care for them.
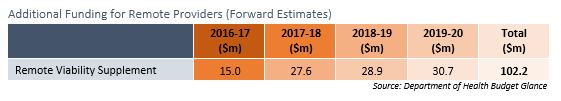
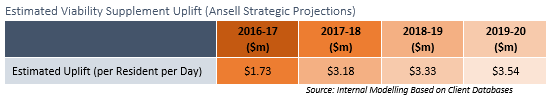
Small Additional Funding Allocations Swallowed by Funding Cuts
Treasurer Scott Morrison states that “savings arising from better targeting of the funding that aged care providers receive will provide the ability to introduce new aged care initiatives and help meet the continued growth in aged care funding overall.”
It appears, however, that only $102 million has been allocated to the providers of care to improve aged care services. This appears somewhat tokenistic given the scale of the cuts and the magnitude of the funding shortfall in regional and remote areas.
The $102 million will be allocated over four years to target the aged care viability supplement more effectively to areas of greatest need by replacing the current outdated remoteness classification system with the more up to date Modified Monash Model. The model is currently used in other health environments and will bring the viability supplement assessment process into line with other health programs. The effect of the supplement, however, will be diluted across residential care, home care and multi-purpose services throughout Australia resulting in a minimal spend on residents.
Critical Implication of the Proposed Changes
The analysis above demonstrated three critical impacts that will follow if the proposed changes to Complex Care funding:
- Sector Investment and Viability – The financial impact of the funding cuts on providers will undermine the viability of the sector. The providers who care for those with the most profound care needs will be affected more than those providers who elect to admit residents with lower complex care needs. The cuts come at a time when investment in aged care services is paramount to address the demands of a rapidly ageing population. It also comes at a time when the prevalence of disability amongst the elderly rise. Homes are increasingly caring for residents who have increased complex care needs relating to longer longevity and multiple comorbidities such as heart disease, diabetes, obesity, chronic pain and dementia.
- Displacement of Residents with Chronic Disease and High Care Needs – By reducing funding for the care of complex residents with the most costly care needs, providers will be less inclined to admit those who are those most in need of residential aged care services. Our experiences of international markets, including New Zealand, has demonstrated the marginalisation or exclusion of residents by providers who are not appropriately compensated for their care. This may result in the displacement of residents into acute care settings.
- Treatment of Suffering – Providers will be less able to address the symptoms of disease within their resident population. The Aged Care Act precludes providers from charging residents for Specified Care and Services. Without appropriate compensation via the ACFI tool, providers will not be able to afford to deliver comprehensive complex care services. Providers will no longer be able to afford allied health led pain treatments, for example, and will increasingly rely on medications to assist with the treatment of chronic pain.
It is critical that the aged care and broader healthcare sector work collaboratively with Government to ensure that these changes do not proceed.