Budget Impact on Residential Care

The 2016-2017 budget impact on residential care
Treasurer Scott Morrison’s 2016-17 budget focuses on long term growth, taxation reform and “cutting unnecessary waste” that “keeps us on a sustainable path to bring the budget back into balance”. It appears that aged care is the focus of “unnecessary waste” with Morrison stating that the government is refining aged care funding to address unsustainable spending.
Health Minister Sussan Ley says the measures are part of the Government’s ongoing commitment to aged care reform. It’s about “putting consumers, not the aged care provider, in charge of their later years”, she said. There appears little, however, in the budget that will provide more funding or choice for consumers.
Cuts to ACFI
The Government says expenditure on the Aged Care Funding Instrument (ACFI) would be expected to blow out by $3.8 billion over the next four years without action. The response is significant with amendments to “certain aspects” of the ACFI funding model aimed to “stabilise higher than expected growth”. The Government hopes that the cuts will bring the ACFI funding back into the budgeted growth trend so that “funding grows at a responsible and sustainable rate”.
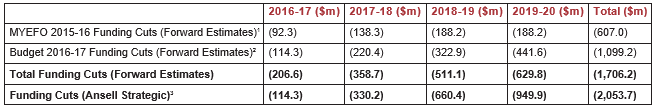
The budget claw back, announced in Budget 2016-17 of $1.1 billion, is exclusive of funding cuts announced in February 2016 through the MYEFO of $607 million, creating an aggregate reduction of $1.71 billion over the next four years.
Following the Federal Budget, the Department of Health released details of the ACFI clawback. Changes focus on the Complex Health Care (CHC) domain. CHC includes medication assistance, pain treatments and other care interventions for the most frail and unwell residents living in residential care. The changes will be implemented in two stages over the coming six months.
On July 1, 2016 changes to the scoring matrix will push a large number of new or reclassified residents who would have previously been classified as requiring high care into the medium care classification.
The January 1, 2017 changes are more profound. Significant changes to the scoring of medication assistance will result in most new or reclassified residents moving from a high to a medium classification. Changes to the scoring and eligibility requirements for CHC treatments, including blood pressure measurements, complex pain treatments and the treatment of oedema, will also see large numbers of residents being classified lower than they would have been previously under the current funding arrangements.
Based on the announced changes to the CHC Domain, Ansell Strategic estimate that the proposed changes to the ACFI Instrument will deliver funding cuts of almost $350 million more than projected by the Government. Our analysis indicates that funding claw backs to providers will be in excess of $2 billion over the next four years alone. As the proposed changes are permanent, there will be long term ramifications for the most vulnerable residents and the providers that care for them. Funding Cuts (Forward Estimations vs. Ansell Strategic Projections)
Within an ageing population, adjustments will be required over time to balance the obligation of funding from taxpayers to consumers. However, these changes are one sided and the impacts will be felt by the providers and the people they care for. An average 80-bed home will lose $439,000 in funding each year following the change.
Small additional funding allocations
Morrison states that “savings arising from better targeting of the funding that aged care providers receive will provide the ability to introduce new aged care initiatives and help meet the continued growth in aged care funding overall.”
The Government will provide $102 million over four years to target the aged care viability supplement more effectively to areas of greatest need by replacing the current outdated remoteness classification system with the more up to date Modified Monash Model. The model is currently used in other health environments and will bring the viability supplement assessment process into line with other health programs.
The increases in rural and remote funding appears somewhat tokenistic given the scale of the cuts and the magnitude of the funding shortfall in regional and remote areas.
Impact on care and viability
We believe that providers will be less able to address the symptoms of disease within their resident population following the funding cuts. The Aged Care Act precludes providers from charging residents for Specified Care and Services. Without appropriate compensation via the ACFI tool, providers will not be able to afford to deliver the same comprehensive complex care services. Providers are already saying that they will no longer be able to afford allied health led pain treatments and will increasingly rely on medications to assist with the treatment of chronic pain.
By reducing funding for the care of complex residents with the most costly care needs, providers will be less inclined to admit those who are most in need of residential aged care services. Our experiences of international markets, including New Zealand, has demonstrated the marginalisation or exclusion of residents by providers who are not appropriately compensated for their care. This may result in the displacement of residents into acute care settings.
Industry players are stating that the financial impact of the funding cuts on providers will undermine the viability of the sector. The providers who care for those with the most profound care needs will be affected more than those providers who elect to admit residents with lower complex care needs.
The cuts come at a time when investment in aged care services is paramount to address the demands of a rapidly ageing population. It also comes at a time when the prevalence of disability amongst the elderly rises. Homes are increasingly caring for residents who have increased complex care needs relating to greater longevity and multiple comorbidities such as heart disease, diabetes, obesity, chronic pain and dementia.